Researchers Uncover New Insights Into Collateral Blood Flow in CTEPH Patients
Written by |
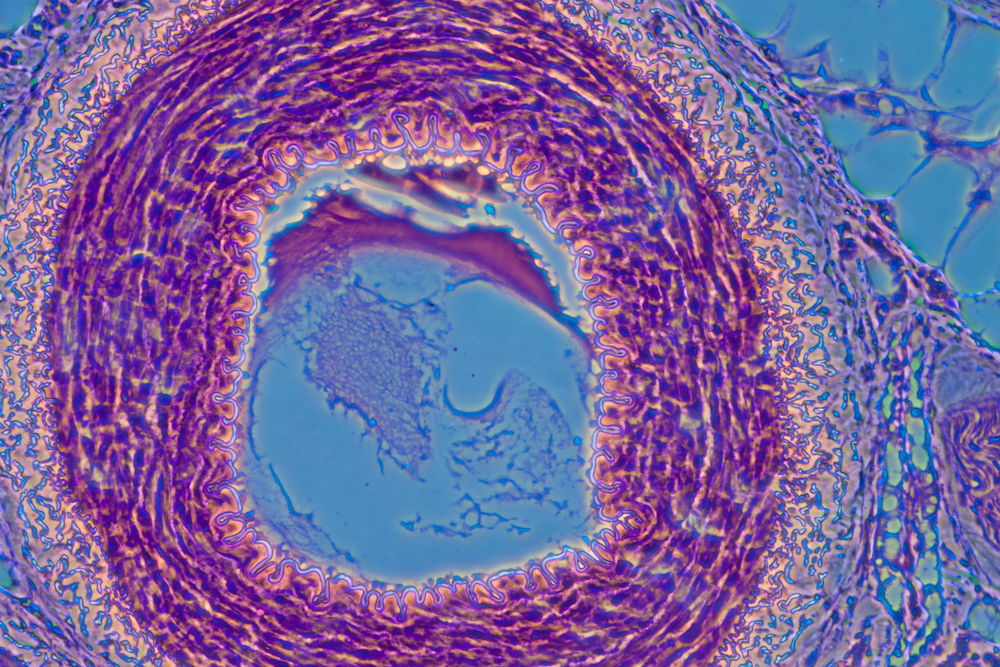
As the supplier of the body’s blood, the heart must also supply its own blood to keep itself nourished and oxygenated. The heart’s blood supply comes from the coronary arteries, which receive oxygenated blood from the pulmonary veins. Normally, the heart receives enough oxygenated blood, but with chronic thromboembolic pulmonary hypertension (CTEPH) is present, a clot may obstruct blood flow.
Fortunately, the body has a “plan B” for ensuring the heart receives an adequate blood supply, and this mechanism is known as collateral blood flow. Collateral blood flow describes a redundant flow of blood in which branches between adjacent blood vessels bypass a blockage in another vessel in order to supply enough oxygenated blood to tissue, such as the heart, downstream of the blockage. When collateral blood flow acts to supply blood to the heart, the vessels are known as coronary artery-pulmonary artery collaterals.
The prevalence and predictors of coronary artery-pulmonary artery collaterals in CTEPH are not well understood. Due to the fact that such an important, life-saving mechanism is important to understand, a team of researchers from the University of California, San Diego investigated coronary artery-pulmonary artery collaterals in CTEPH patients. Their research was published in an article titled, “Prevalence of Coronary Artery-Pulmonary Artery Collaterals in Patients with Chronic Thromboembolic Pulmonary Hypertension,” in the journal Pulmonary Circulation.
The team studied 259 patients with CTEPH to identify coronary artery-pulmonary artery collaterals. In order to detect the presence of these vessels, the researchers evaluated coronary angiograms, in which CTEPH patients had a special X-ray contrast dye injected through a catheter into the arteries in order for their arteries to show up on X-rays. Looking at these X-rays, the researchers noted that 10.8% of CTEPH patients had coronary artery-pulmonary artery collaterals, whereas only one control subject (0.4%) had collaterals. When comparing CTEPH patients with and without collaterals, the CTEPH patients more frequently had total occlusion of either the right or left main pulmonary artery or lobar arteries, indicating that the collaterals formed to rescue blood flow to the heart.
The researchers believe that identifying the presence of collaterals in CTEPH patients hold diagnostic and prognostic value. Since collaterals indicated greater pulmonary artery obstructions, a coronary angiogram may be used to help detect CTEPH in suspect patients.



