SSc-PH May Show Increase in Damaged Blood Vessel Biomarker EMPs
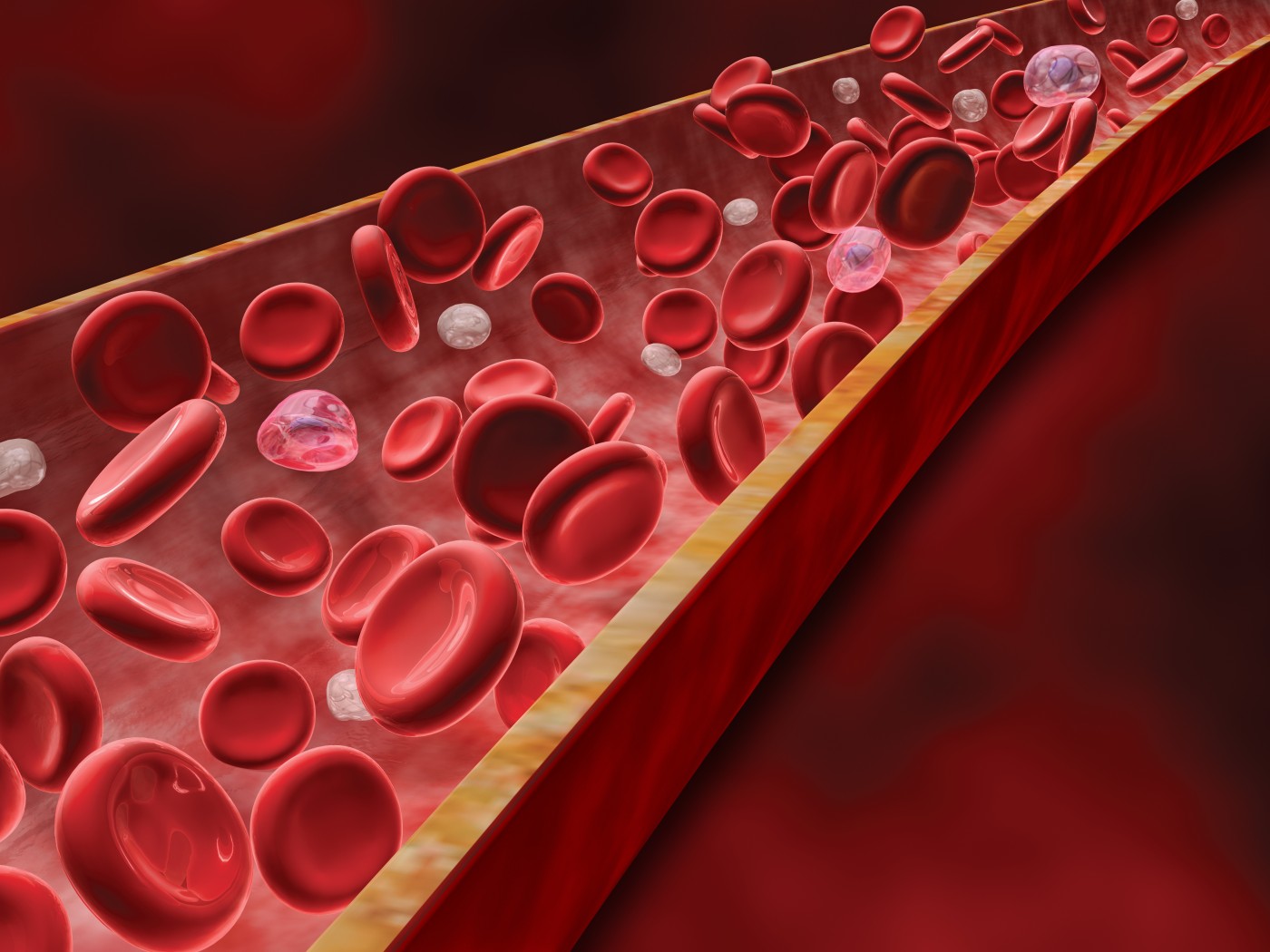
 Tiny biomarkers for pulmonary hypertension in patients with systemic sclerosis (SSc) may be floating around affected individuals’ bloodstreams. Matthew R. Lammi, MD, of Louisiana State University Health Sciences Center in New Orleans is heading a clinical trial to evaluate the presence of endothelial microparticles (EMPs) in SSc patients with or without pulmonary hypertension and compare the results between groups and against age-matched, healthy control participants.
Tiny biomarkers for pulmonary hypertension in patients with systemic sclerosis (SSc) may be floating around affected individuals’ bloodstreams. Matthew R. Lammi, MD, of Louisiana State University Health Sciences Center in New Orleans is heading a clinical trial to evaluate the presence of endothelial microparticles (EMPs) in SSc patients with or without pulmonary hypertension and compare the results between groups and against age-matched, healthy control participants.
Since SSc is characterized by fibrosis and inflammation in the skin, organs, and blood vessels, afflicted patients tend to see an increased risk for pulmonary hypertension as a result of narrowed blood vessels leading to the lungs. Damage to the blood vessel lining — the endothelium — releases EMPs into circulation, and it is natural to assume there is an increased level of EMPs in SSc patients with pulmonary hypertension. The clinical trial, “Endothelial Microparticles in Systemic Sclerosis Pulmonary Hypertension,” seeks to test this hypothesis and is currently recruiting participants.
[adrotate group=”4″]
In addition to the main goal of identifying EMPs in SSc/pulmonary hypertension patients’ blood, another goal attempts to answer “the chicken or the egg” question: are EMPs really the cause of blood vessel damage? To answer this question, the researchers will isolate EMPs from SSc patient blood and apply them to human endothelial cells grown in vitro to identify negative effects.
To be more specific to the EMPs studied in this trial, the researchers are looking to identify the proportion of EMPs positive for VE-cadherin, PECAM, and E-selectin, three major molecules that decorate the cell membrane of endothelial cells. Blood collection will occur only once for a patient, on the first day of visiting the trial clinic.
[adrotate group=”3″]
Finally, the researchers are interested in treating damaged endothelial cells with mycophenolate mofetil (MMF), also known as CellCept, which is a treatment for individuals receiving an organ transplant. This drug agent may have an effect on EMP levels, and decreasing EMP may increase the livelihood of damaged cells. In the future, MMF may be developed as a new treatment for vascular disease, but these initial preclinical studies are required.
The results of this study will be important for determining possible clinical factors to accurately predict pulmonary hypertension in patients with SSc.







