Systemic Sclerosis Patients with High Pulmonary Artery Pressure May Have Increased Mortality
Written by |
Systolic pulmonary artery pressure greater than 36 mm Hg reduced survival in patients with systemic sclerosis (SSc) according to an article entitled “Value of Systolic Pulmonary Arterial Pressure as a Prognostic Factor of Death in the Systemic Sclerosis EUSTAR Population,” published September 2014, in the journal Rheumatology.
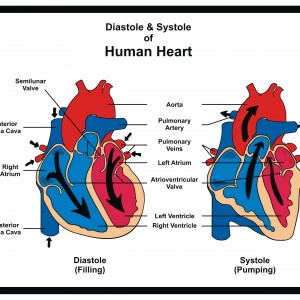 Both systolic and diastolic pressure are used to measure heart function. The systolic pressure refers to when the heart has contracted and is pushing blood through the circulatory system.
Both systolic and diastolic pressure are used to measure heart function. The systolic pressure refers to when the heart has contracted and is pushing blood through the circulatory system.
[adrotate group=”4″]
SSc is a connective tissue disease affecting many different systems within the body, including the lungs. It is characterized by diseased blood vessels and fibrosis — the thickening and scarring of connective tissue. Pulmonary arterial hypertension (PAH) refers to abnormally high blood pressure in the lung arteries is one of the most severe problems that can occur in SSc. It is also a main cause of death in people with SSc, occurring in about 10% of those with SSc. About half of people with SSc die within three years of developing pulmonary arterial hypertension.
An international group of researchers, led by Eric Hachulla from the Department of Internal Medicine, Lille Nord University, France, analyzed results from the European League Against Rheumatism Scleroderma Trial and Research (EUSTAR) database for 1,476 individuals with sSSc. They took measurements between January 2005 and December 2011, including ecocardiography. Echocardiography refers to the use of ultrasound waves to investigate the action of the heart and blood function. The scientists collected additional data including disease symptoms, history of renal crisis and co-existing separated medical conditions and studied the participants for a duration of up to 2 years.
[adrotate group=”3″]
The researchers used a systolic pulmonary artery pressure (sPAP) of more than 30 mm Hg as a reference point. mmHg means millimeters of mercury and is a way to measure blood pressure. They found that the risk of death increased substantially when the sPAP was between 30 mm Hg and 36 mm Hg. The death risk more then doubled for sPAP between 36 mm Hg and 40 mm Hg, and was almost four times greater for sPAP between 40 mm Hg and 50 mm Hg, and up to ten times greater if sPAP was higher than 50 mm Hg.
The authors concluded that, “an estimated sPAP 36 mmHg at baseline echocardiography was significantly and independently associated with reduced survival.”
The scientists noted that the measurement could have implications for the clinical management of SSc, noting ” our data support the idea that in routine clinical management of SSc patients, sPAP ≥36 mmHg should be seen as a red flag indicating a high risk of death, resulting in immediate RHC to identify or exclude PH.”



