Acetylcholine levels linked with PH symptom severity, prognosis: Study
Patients have higher risk of mortality, heart failure, worsening symptoms
Written by |
People with pulmonary hypertension (PH) and high blood acetylcholine (ACh) levels show more severe symptoms and a poorer prognosis than those with lower ACh levels, a single-center study in China suggests.
ACh is a neurotransmitter, a chemical messenger that allows nerve cells to communicate throughout the body. It’s involved in several important functions, including regulating heart function and blood pressure. PH patients with higher ACh blood levels were at a higher risk of mortality, heart failure, and worsening symptoms, researchers found.
“Our study first demonstrated the potential biomarker role of ACh in PH, indicating its value in disease management,” they wrote in “Circulating acetylcholine serves as a potential biomarker role in pulmonary hypertension,” which was published in BMC Pulmonary Medicine.
PH is a progressive condition marked by high blood pressure in the pulmonary arteries, the blood vessels that supply the lungs. Its main symptoms include shortness of breath, fatigue, dizziness, and chest pain. Increased blood pressure in the lungs means the right side of the heart must work harder to pump blood through the arteries, which may lead to heart failure.
Previous studies have implicated ACh in pulmonary circulation, with increased ACh levels in the patients’ right ventricle, the part of the heart that pumps blood into the lungs, indicating it may be involved in PH-causing mechanisms.
“However, to date, the relationship between [blood] ACh levels and disease conditions and PH patients’ prognosis has not been elucidated,” wrote researchers in China, who studied 408 PH patients over an average of 2.5 years.
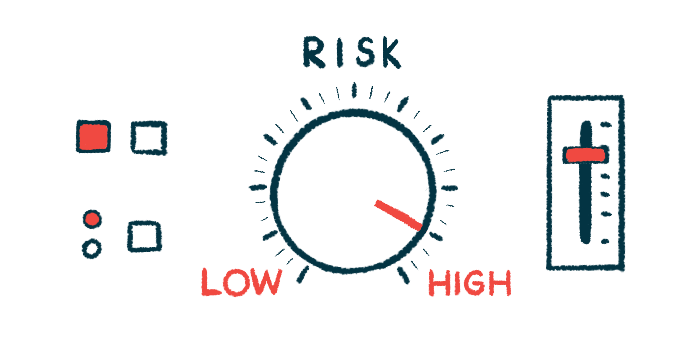
Risks of higher acetylcholine levels
Patients were mainly women (68.1%) and had a mean age of 43.1. Most had pulmonary arterial hypertension (294), caused by the narrowing of pulmonary arteries, and 106 had chronic thromboembolic pulmonary hypertension (CTEPH), caused by blood clots. The remaining eight had other PH types.
The study’s primary goal was to evaluate a disease composite outcome including death/lung transplant, heart failure, and worsening of PH symptoms. These clinical outcomes were also analyzed separately.
During the follow-up, 133 patients had primary outcomes — 130 experienced symptoms worsening, 106 had heart failure, and 58 died. Patients with ACh blood levels above 0.76 micromol (mcmol)/L were at a higher risk for these outcomes than those whose levels were lower.
Participants were then divided into high and low ACh blood levels, with 0.76 mcmol/L being the cutoff value. The higher ACh group was made up of older patients, a higher proportion of men, and had significantly higher mean values of heart pressure and pulmonary vascular resistance, or resistance to blood flow, than the low ACh group.
Moreover, those in the high ACh group were more likely to have severe symptoms and a poor prognosis: they had a worse World Health Organization Functional Class, a measure of PH symptom severity, and a lower six-minute walk distance, an indicator of exercise capacity.
They also had higher levels of NT-proBNP, which may be a sign of heart failure, and had echocardiography parameters indicative of worse heart function. An echocardiogram allows the heart’s structure to be visualized.
After adjusting for possible confounding factors such as age, PH type, or coexisting disorders patients with higher ACh levels remained at an elevated risk of mortality, heart failure, and symptom worsening than those with lower levels.
“Importantly, our results indicated the potential use of ACh as a [blood]-based biomarker to monitor PH progression, but further confirmation is needed through large-scale prospective cohort studies,” the researchers wrote.