Winrevair (sotatercept-csrk) for pulmonary arterial hypertension
What is Winrevair for pulmonary arterial hypertension?
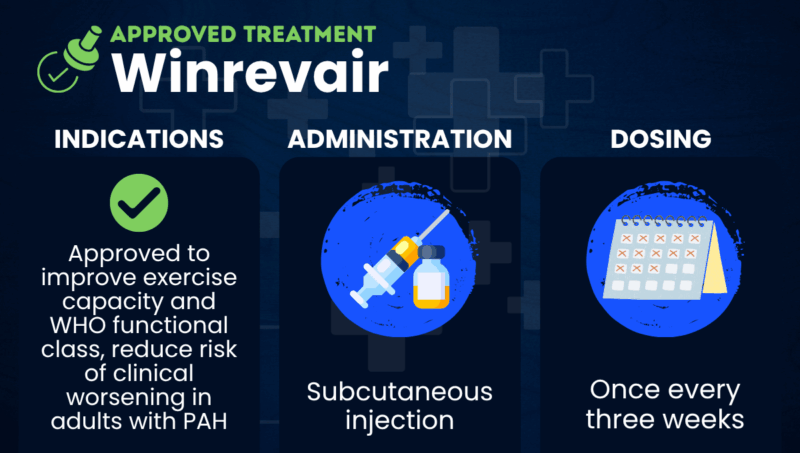
Winrevair (sotatercept-csrk) is an injection therapy for adults with pulmonary arterial hypertension (PAH), approved in the U.S. to improve exercise capacity and World Health Organization (WHO) functional class, and to reduce the risk of clinical worsening events.
In PAH, the pulmonary arteries that supply blood to the lungs become narrow, restricting blood flow and raising pressure. The abnormal growth of endothelial and smooth muscle cells that line the pulmonary arteries is part of this constriction process.
Winrevair works by inhibiting the activation of the activin signaling pathway, which plays a central role in this abnormal cell growth. Specifically, it binds to growth factor molecules involved in the pathway and prevents them from sending signals to those cells.
By rebalancing cell growth, the medication should help widen the pulmonary arteries and improve blood flow through them, easing disease symptoms and slowing PAH progression.
Given via under-the-skin (subcutaneous) injections, Winrevair is marketed by Merck. Ongoing clinical trials are assessing the medication for other indications, including in pediatric PAH or people with other types of pulmonary hypertension (PH).
Therapy snapshot
| Brand name | Winrevair |
| Chemical name | Sotatercept-csrk |
| Usage | Used to improve exercise capacity and WHO functional class, and to reduce the risk of clinical worsening in adults with PAH |
| Administration | Subcutaneous injection |
Who can take Winrevair?
In the U.S., Winrevair is approved for adults with PAH (WHO Group 1) to improve exercise capacity and WHO functional class, as well as to reduce the risk of clinical worsening events, including hospitalization for PAH, lung transplantation, and death.
No contraindications are listed for its use.
In the European Union, Winrevair is approved for use in combination with other PH therapies for adults with PAH in WHO functional class II or III, corresponding to moderate or marked limitations of physical activity.
How is Winrevair administered?
Winrevair is given by subcutaneous injections into the stomach or upper thigh once every three weeks. With proper training on how to prepare and inject the medication, patients or caregivers can administer Winrevair at home without medical supervision.
The recommended starting dose is 0.3 mg/kg, which will be increased to a target maintenance dose of 0.7 mg/kg if blood tests suggest it is safe to do so. The medication comes as a powder that must be dissolved in sterile water before use.
Patients will undergo blood tests before each of the first five doses of Winrevair, or longer if necessary, and periodically thereafter. These tests are to make sure the patient has safe levels of hemoglobin, which is the oxygen-carrying protein in red blood cells, and platelets, the cell fragments involved in blood clotting. If the tests detect abnormalities, scheduled injections of Winrevair may need to be delayed.
Winrevair in clinical trials
The primary clinical trial that supported the U.S. approval of Winrevair was the Phase 3 STELLAR trial (NCT04576988), which included 323 adults with PAH in WHO functional class II or III. Participants received Winrevair or a placebo in addition to their background PAH therapy for 24 weeks (about six months). Results showed that, compared with the placebo, Winrevair:
- significantly improved exercise capacity, increasing the distance walked in six minutes by 40.8 meters compared with the placebo
- was associated with higher rates of improvement in WHO functional class (29% vs. 14%)
- lowered the risk of clinical worsening or death by 84%.
Supportive data also came from ZENITH (NCT04896008), a Phase 3 study that involved 172 participants with advanced PAH (WHO functional class III or IV). Among these high-risk patients, Winrevair was associated with a 76% lower risk of death, lung transplantation, or hospitalization compared with a placebo.
Data from a third Phase 3 trial called HYPERION (NCT04811092) showed similar clinical benefits when Winrevair was used in adults recently diagnosed with PAH who were at a medium or high risk of disease progression.
Ongoing studies are evaluating Winrevair in additional PH populations, including:
- MOONBEAM (NCT05587712), a Phase 2 trial testing Winrevair in children, 1 to 17 years old, with PAH
- CADENCE (NCT04945460) and its extension study, HARMONIZE (NCT06814145), which include adults with combined postcapillary and precapillary pulmonary hypertension, a type of PH caused by left-sided heart disease.
Winrevair side effects
The most common side effects of Winrevair include:
- infections
- headache
- rash
- nosebleeds (epistaxis)
- damaged blood vessels visible under the skin (telangiectasias or spider veins)
- diarrhea
- dizziness
- skin redness (erythema)
- gum bleeding
- increased levels of hemoglobin.
Warnings for less common but potentially severe side effects include:
- high concentration of red blood cells (erythrocytosis), which can increase the risk of blood clotting complications or hyperviscosity syndrome, in which the blood is unusually thick and flows slowly
- severe decreases in platelet counts, which could increase the risk of bleeding
- serious bleeding events, which are more likely if platelet counts are low or a person is also using certain other medications
- potential harm to a developing fetus
- impaired fertility for men and women.
Periodic blood tests will monitor changes in hemoglobin levels and platelet counts that could cause side effects. If serious bleeding is occurring, Winrevair shouldn’t be administered.
Female patients of reproductive potential should use an effective method of contraception during treatment with Winrevair and for four months after the final dose.
Pulmonary Hypertension News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.

 Fact-checked by
Fact-checked by