Activation of PPAR-gamma May Be Potential Strategy Against PAH, Other Disorders, Study Suggests
Written by |
Activation of a molecule called PPAR-gamma may be a future strategy to prevent pulmonary arterial hypertension (PAH) and other cardiovascular/pulmonary diseases, a study suggests.
Findings were reported in the study, “PPARγ agonist pioglitazone reverses pulmonary hypertension and prevents right heart failure via fatty acid oxidation,” published in the journal Science Translational Medicine.
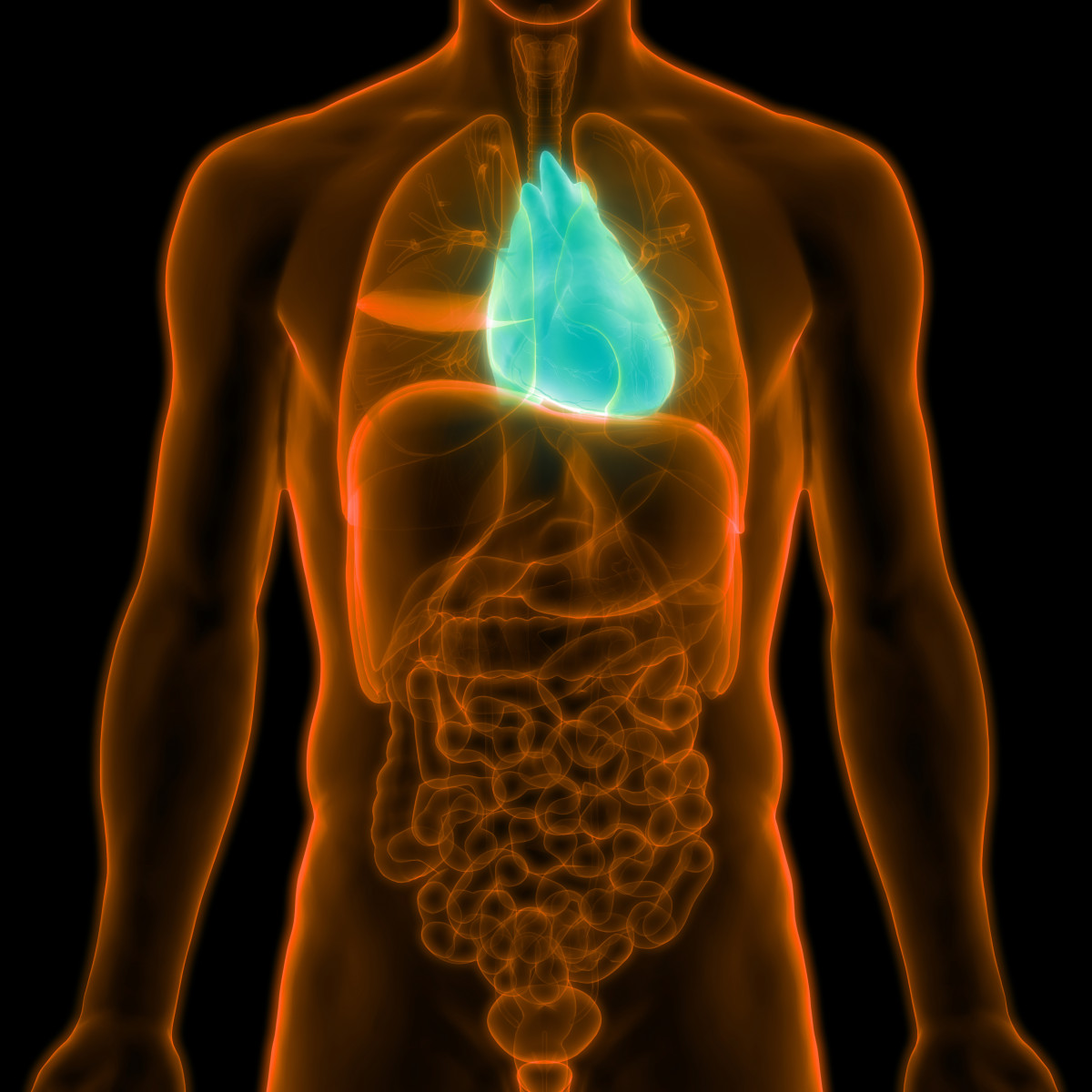
Right ventricular (RV) heart failure is the major cause of death in patients with PAH. Heart failure in PAH involves diverse events, including RV hypertrophy, or thickening; cardiac fibrosis, or scarring; and reduced density of tiny blood vessels.
Abnormal glucose and lipid (fat) metabolism, as well as impaired epigenetic regulation — changes in gene expression that do not involve alterations in the DNA sequence itself — have been proposed as mechanisms involved in both PAH and RV failure. In PAH, the heart, skeletal muscle, and adipose tissue show vascular and metabolic alterations, indicating the disease is not exclusively pulmonary.
Fatty acid oxidation (FAO) produces approximately 70 percent of the ATP — the main source of energy for most cellular processes — used by the heart. Data from animal models suggested that increasing FAO in cardiomyocites — the cells that make up the heart muscle — may be beneficial in preventing heart failure.
Although significant research identified regulatory microRNAs (miRNAs) — small RNA molecules that control gene expression — in muscle cells of the pulmonary artery, little is known about the production of these miRNAs in RV failure, and how they affect fatty acid storage, transport and oxidation.
Research indicates that PPAR-gamma, a key molecule in gene expression related to glucose and fatty acid metabolism, has a protective role in pulmonary artery cells in PAH. PPAR-gamma regulates molecular pathways in vascular smooth muscle cells, as well as other miRNAs, FAO, and glucose metabolism. Of note, switching from FAO to glucose as an energy source may contribute to heart failure in the adult ventricle, the authors said.
These observations led to the hypothesis that PPAR-gamma may be beneficial in heart failure. In fact, previous studies showed that the PPAR-gamma agonist pioglitazone (Pio) improved left ventricular function, and had a positive safety profile.
Researchers in this study showed that in mice with genetically deleted PPAR-gamma, there is lipid accumulation in cardiomyocites, indicative of impaired FAO, and systolic dysfunction — which refers to impaired ventricular contraction.
Using a rat model of PH, the researchers observed that oral treatment with Pio completely reversed severe PAH and vascular remodeling, while preventing RV failure through induction of FAO and maintaining morphology and function of mitochondria — the cell’s power plants. Importantly, Pio also modulated the dysregulated cardiac fibrosis and myocardial contraction.
These effects were mediated by networks of miRNA/messenger RNA (the first product of gene expression, which gives rise to proteins) previously not linked with PAH/RV failure.
Results were replicated in samples from idiopathic PAH patients. The investigators found altered levels of miR-197 and miR-146b in the pressure-overloaded, failing RV; miR-146b and miR-133b in peripheral pulmonary arteries; and miR-133b and miR-146b in plexiform vasculopathy, which refers to complex blood vessel formations originating from remodeled pulmonary arteries.
“Together, [PPAR-gamma]-activating drugs, such as pioglitazone, are promising agents for the treatment and prevention of PAH/RV failure and other conditions associated with altered lipid/glucose metabolism,” the researchers wrote.



